A Radiation Synthetic Combination for Osteosarcoma Local Control: $100,000 annually
Be the sponsor of this project! Osteosarcoma is a disease for which local control can be critical: for tumors in a limb, local control permits

CureFast: Creating a Legacy by Accelerating Childhood Cancer Research: $156,000 annually
Be the sponsor of this project! One in 5 children with cancer will not survive. We propose to address gaps in basic and translational research

Marizomib in Medulloblastoma: $240,000 over 2 years
The goal of this preclinical study is to validate marizomib as a treatment for medulloblastoma.
Dupixent as an anti-metastasis agent for Rhabdomyosarcoma: $240,000 over 2 years
Be the sponsor of this project! What if an FDA-approved dermatitis and asthma medicine could stop rhabdomyosarcoma metastasis? The major goal of this project is
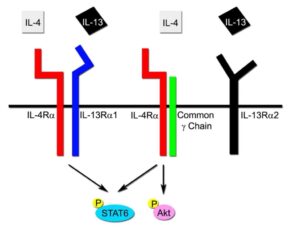
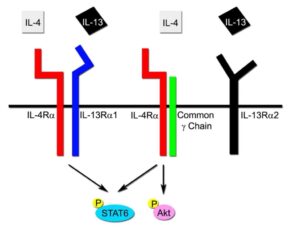
The IL13RA2-HAS2 axis as therapeutic co-targets in DIPG: $249,000 over 2 years
Be the sponsor for this project! We have investigated presence of the IL13RA2 protein in DIPG, and we have shown there is 13 times higher
A Radiation Synthetic Combination for Osteosarcoma Local Control: $100,000 annually
Be the sponsor of this project! Osteosarcoma is a disease for which local control can be critical: for tumors in a limb, local control permits

CureFast: Creating a Legacy by Accelerating Childhood Cancer Research: $156,000 annually
Be the sponsor of this project! One in 5 children with cancer will not survive. We propose to address gaps in basic and translational research

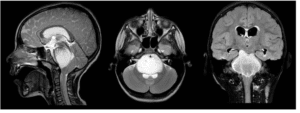
Marizomib in Medulloblastoma: $240,000 over 2 years
The goal of this preclinical study is to validate marizomib as a treatment for medulloblastoma.
Dupixent as an anti-metastasis agent for Rhabdomyosarcoma: $240,000 over 2 years
Be the sponsor of this project! What if an FDA-approved dermatitis and asthma medicine could stop rhabdomyosarcoma metastasis? The major goal of this project is
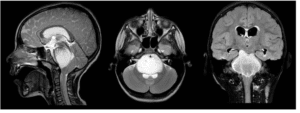
The IL13RA2-HAS2 axis as therapeutic co-targets in DIPG: $249,000 over 2 years
Be the sponsor for this project! We have investigated presence of the IL13RA2 protein in DIPG, and we have shown there is 13 times higher